Iron Deficiency Anaemia
General points
- Please ensure the anaemia is iron deficient before referral to gastroenterology
- Iron deficiency is defined by a low ferritin (biochemistry reports have reference values) and / or low Hb that responds to iron therapy
- Ferritin maybe falsely raised so perform a CRP as well
- The likelihood of a cause being found increases with age and the more severe the anaemia – consider this when deciding routine or urgent or 2 week wait referral
- Dip the urine - 1% have renal tract carcinoma
- Patients with normal Hb but a low ferritin should be referred if age 50 or over
- Please perform a PR examination
Definition of IDA
- Anaemia by local laboratory values and
-
Ferritin < 15 ug/L
- ferritin 15-30 ug/L with a normal CRP or 15-70 mg/L with a raised CRP is an equivocal result - it might be IDA and would warrant a trial of iron
- ferritin > 30 ug/L with a normal CRP or >70 mg/L with a raised CRP is seldom IDA - if in doubt give trial of iron
-
or anaemia responding to iron therapy e.g. ferrous sulphate 200mg bd
- Hb will increase by 1g/dl or more over 2 weeks if the patient is iron deficient
Please refer:
- All men and non-menstruating females
-
Menstruating females only need referral if they have
- GI symptoms or
- age 50 or over or
- strong family history of GI cancer = one first degree relative diagnosed under age 45 or two affected first degree relatives
Referral urgency:
-
Aged 50 or over with unexplained iron deficiency anaemia – refer via the 2ww colorectal service.
Otherwise urgent or routine ERS referral depending on the likelihood of cancer (which increases with age and severity of anaemia)
Investigations prior to referral
- FBC ferritin CRP
- +/- response to iron
- Coeliac serology (anti-TTG antibodies)
- Urinalysis
However please don’t delay an urgent referral awaiting coeliac serology
Treatment
- give iron until Hb normalises and for 3 months thereafter
- then watch FBC 3monthly for a year then yearly
- please see clinical guidance map below for full details
Relapse
- If Hb or MCV drops give iron again as above
- Further GI investigation is only necessary if the Hb cannot be maintained on iron
Upper GI red flags/2ww criteria:
Refer for direct access gastroscopy:
- Dysphagia
-
Aged 55 or over with weight loss AND any of the following:
- Reflux
- Abdominal pain
- Dyspepsia
Refer to the upper GI 2ww service:
- Ultrasound indicates gall bladder cancer
- CT indicates pancreatic cancer
- Ultrasound indicates pancreatic cancer
- Upper abdominal mass consistent with gastric cancer
- Any patient with jaundice
-
Aged 60 or over with weight loss AND any of the following:
- Diarrhoea
- Back pain
- Abdominal pain
- Nausea
- Vomiting
- Constipation
- New onset diabetes
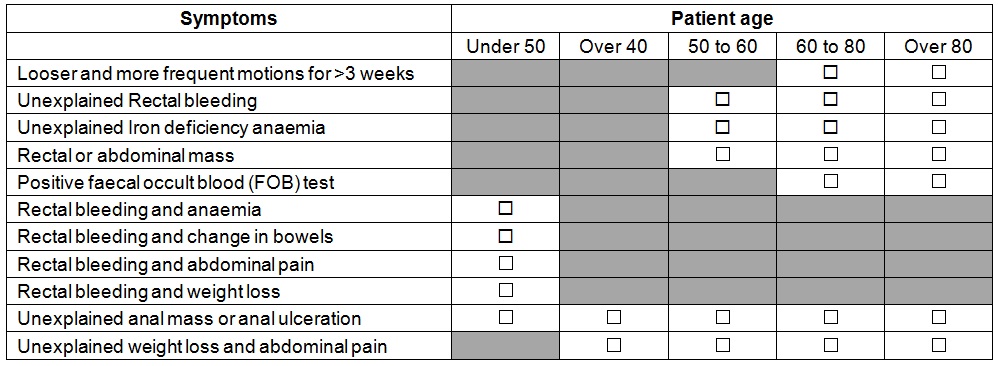
Lower GI cancer:
References:
Clinical Knowledge Summaries (CKS). Anaemia – Iron Deficiency. Newcastle Upon Tyne: CKS; 2009.
British Society of Gastroenterology (BSG). Guidelines for the management of iron deficiency anaemia. London: BSG; 2005.
