CKD
Definition of CKD
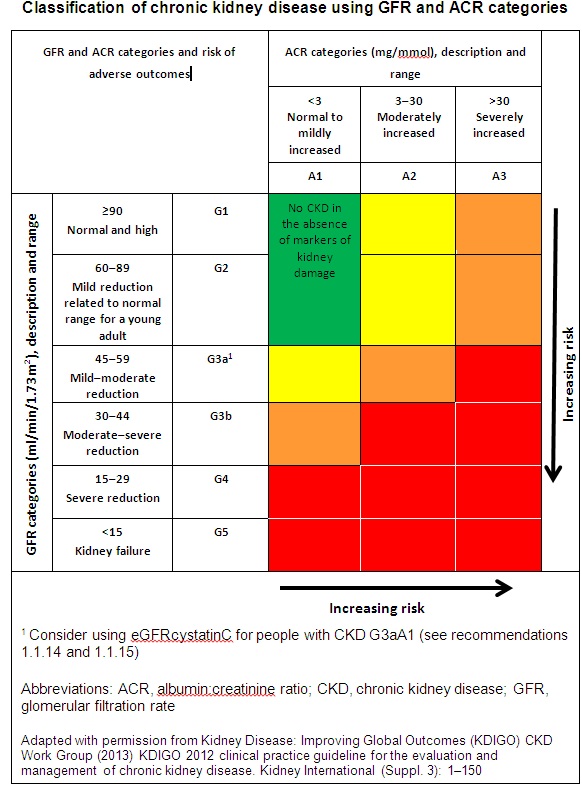
NICE defines CKD as abnormalities of kidney function or structure present for more than 3 months, with implications for health. This includes all people with markers of kidney damage and those with a glomerular filtration rate (GFR) of less than 60 ml/min/1.73 m2 on at least 2 occasions separated by a period of at least 90 days
Offer a renal ultrasound scan to all people with CKD who:
- have progression of CKD
- have visible or persistent invisible haematuria
- have symptoms of urinary tract obstruction
- have a family history of polycystic kidney disease and are aged over 20 years
- have a GFR of less than 30 ml/min/1.73 m2 (GFR category G4 or G5)
Accelerated progression of CKD is defined as
- a sustained decrease in GFR of 25% or more and a change in GFR category within 12 months or
- a sustained decrease in GFR of 15 ml/min/1.73 m2 per year.
Take the following steps to identify the rate of progression of CKD:
- Obtain a minimum of 3 GFR estimations over a period of not less than 90 days.
- In people with a new finding of reduced GFR, repeat the GFR within 2 weeks to exclude causes of acute deterioration of GFR – for example, acute kidney injury or starting renin–angiotensin system antagonist therapy
Be aware that people with CKD are at increased risk of progression to endstage
kidney disease if they have either of the following:
- a sustained decrease in GFR of 25% or more over 12 months or
- a sustained decrease in GFR of 15 ml/min/1.73 m2 or more over 12 months.
When assessing CKD progression, extrapolate the current rate of decline of
GFR and take this into account when planning intervention strategies,
particularly if it suggests that the person might need renal replacement therapy
in their lifetime.
Monitoring CKD
NICE recommends use table 2 to guide the frequency of GFR monitoring for people with, or at risk of, CKD, but tailor it to the person according to:
- the underlying cause of CKD
- past patterns of eGFR and ACR (also be aware that CKD progression is often nonlinear)
- comorbidities, especially heart failure
- changes to their treatment (A2RB, NSAIDs and diuretics)
- intercurrent illness
%20for%20people%20with,%20or%20at%20risk%20of,%20CKD.jpg)
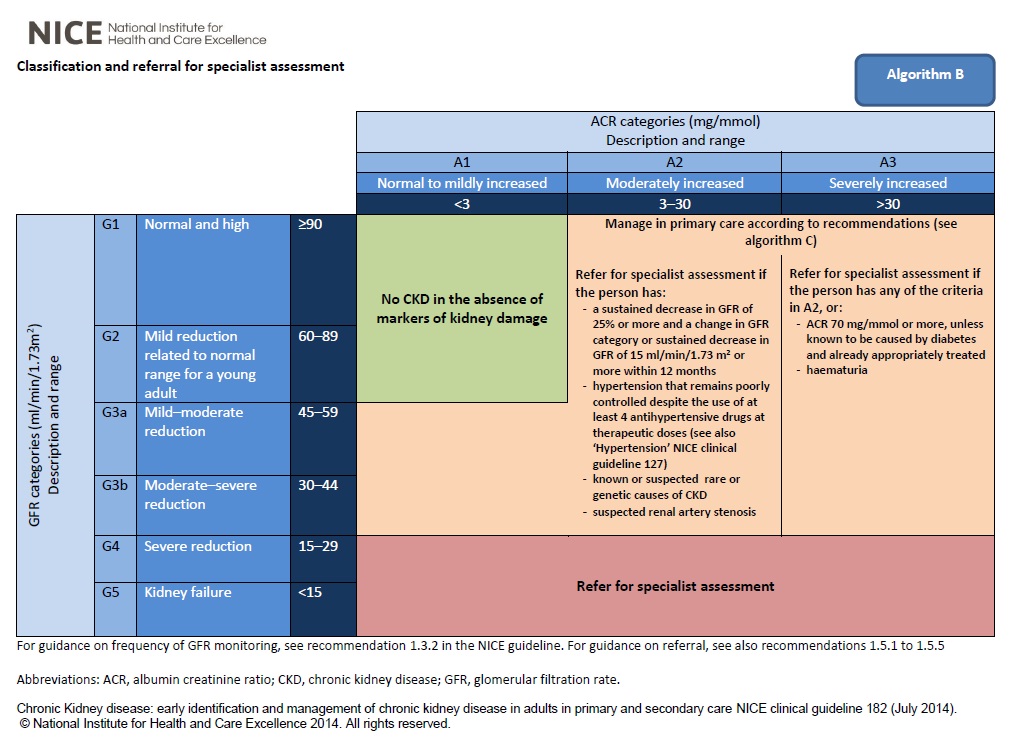
When to refer
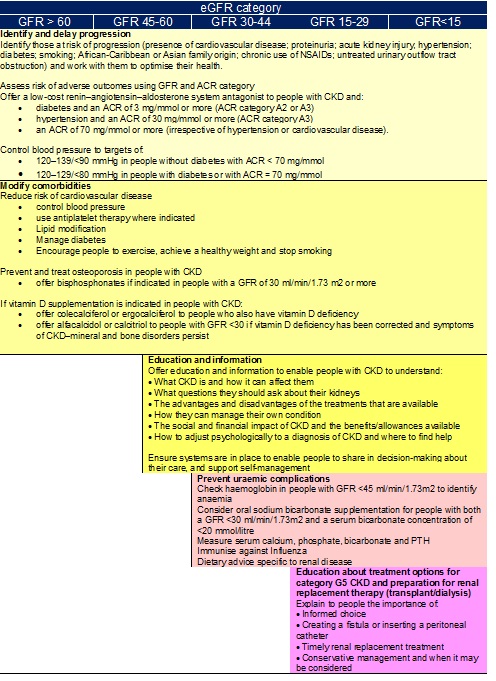
Clinical priorities at each stage of CKD